Presentation:
Leigh, a 36 year old computer engineer presented with gradually worsening low back pain. This had been going on for approximately 2-3 years. There’s nothing particularly unusual here. He has a sedentary job that involves a lot of sitting.
Symptoms:
Leigh’s pain was described as “a deep, dull, ache”. While largely localised to the lumbo-sacral junction, it had recently begun to spread to the thoraco-lumbar region. This starts to raise some concern. As soon as any pain begins to spread we need to start paying close attention. As we all know, the most common spread pattern for low back back pain tends to be down, not up. There are exceptions to every rule but let’s start looking at the most common causes of this. There was no peripheralisation, Valsalva was negative and there were no Cauda Equina symptoms. All happy here.
History:
The symptoms began very gradually over the previous 2-3 years. There was no obvious etiology and he had suffered no trauma. He had no prior history of illness but had been recently experiencing occasional fevers and bouts of photophobia. His GP had assessed this to be due a mild viral infection. OK, here we go. Fever and photophobia are usually indications of an inflammatory process so we’d better start looking in that corner.
He was on no regular medication.
Examination:
Leigh’s cervical ranges of motion were all normal and pain free. His lumbar ranges of motion were slightly reduced by stiffness in the mid-range with a soft end-range restriction due to pain. This was largely around the lumbo-sacral region. This pattern of restriction is not what I’d expect from a biomechanical issue such a subluxation or disc injury. It’s beginning to look more like an inflammatory state.
Orthopaedic:
All orthopaedic tests were unremarkable with the exception of the Supported Adam’s Test (Belt Test) which indicated some restriction in the sacro-iliac joints. This is one of my favourite quick tests that I include in every examination. In this case it was pointing clearly at an SIJ issue more than lumbo-sacral. Combining the Supported Adam’s with pattern of pain restriction makes it look more and more like an inflamed SIJ – but from what?
Neurological Examination:
All cranial nerves tests were normal and bilaterally equal, as were all peripheral neurological tests.
What Is Your Provisional Diagnosis?
Ankylosing Spondylitis based on the location, spread pattern, fevers and photophobia
If You Have A Differential Diagnosis or Diagnoses, What Is It (or They)?
Enteropathic Arthritis – ruled out because neither he nor anyone in his family have or had Crohn’s disease, ulcerative colitis, inflammatory bowel diseases, Whipple’s disease, Celiac disease, or intestinal bypass surgery
Psoriatic Arthritis – ruled out because neither he nor anyone in his family have or had Psoriasis
What Further Tests (if any) Would You Do?
Blood Tests & Results:-
~Genetic Marker~
HLA-B27 (Positive in ~80–90% of people with ankylosing spondylitis but not diagnostic on it’s own as it’s often present in those without the disease)
Positive
~Inflammatory Markers~
ESR (Erythrocyte Sedimentation Rate)
32 mm/hr
(Reference: 0–20 mm/hr)
Elevated; commonly seen in inflammatory disorders including early AS.
CRP (C-Reactive Protein)
12 mg/L
(Ref: <5 mg/L)
Mild elevation consistent with inflammation.
~Others~
CBC (Complete Blood Count) – may show mild anemia of chronic disease, especially Crohn’s or IBS.
All normal except:
Hematocrit – 40% (Ref: 41%-53%)
Platelets – 345 ×10⁹/L (Ref: 150–400) Mildly elevated (common with inflammation)
RF (Rheumatoid Factor) – usually negative in AS; helps distinguish from rheumatoid arthritis. Negative
Anti-CCP antibodies – typically negative; also helps rule out RA Negative
Imaging:-
When Leigh first presented in 1990 MRI was extremely scarce in Australia and was not accessible by Chiropractors, so the only imaging available was X-ray. These days we would almost always go straight to MRI because it shows far more intra-osseous detail, especially œdema.
Here’s the key X-ray image:
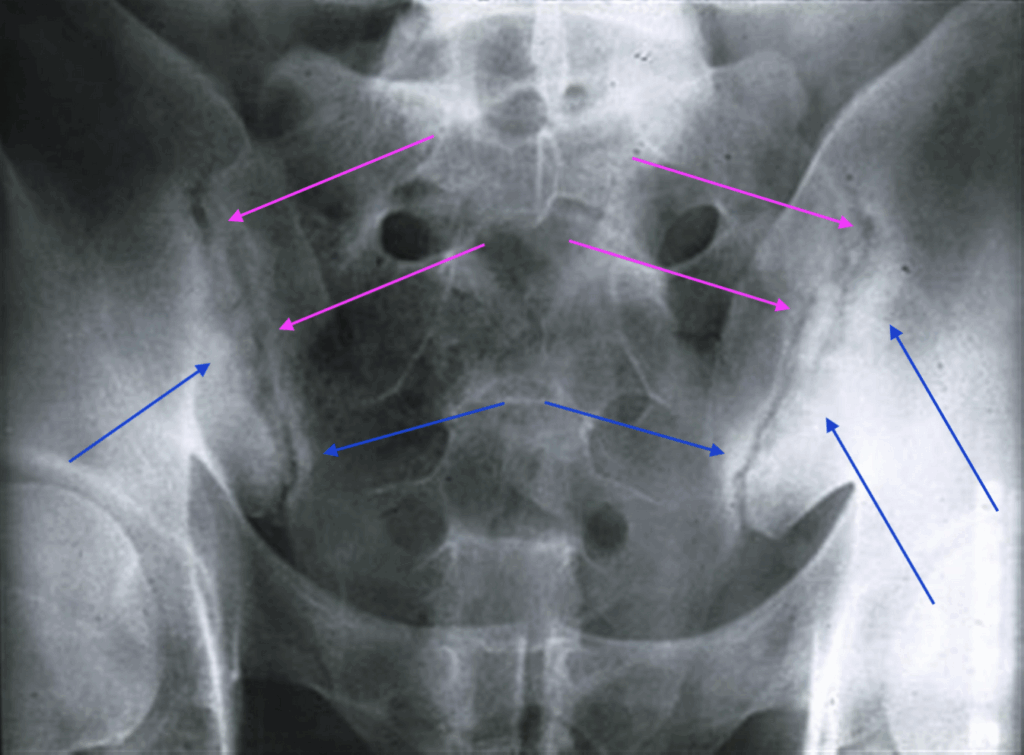
The MAGENTA arrows show bone condensation and the BLUE arrows show increased joint irregularity – common findings in AS
The combination of History, Age, Gender, Symptoms, Orthopaedic Tests, Blood Test results and Radiographic results confirmed the diagnosis of early stage Ankylosing Spondylitis.
Is This A Chiropractic Case?
Yes, it was then and still is.
When we started seeing Leigh, apart from the restriction mentioned above, he still had a relatively full range of motion. And despite the low back pain he was still able to enjoy an active and fulfilling life. He was concerned that it was getting worse and he wanted a diagnosis, some form of help and a prognosis. We were able to give him all three.
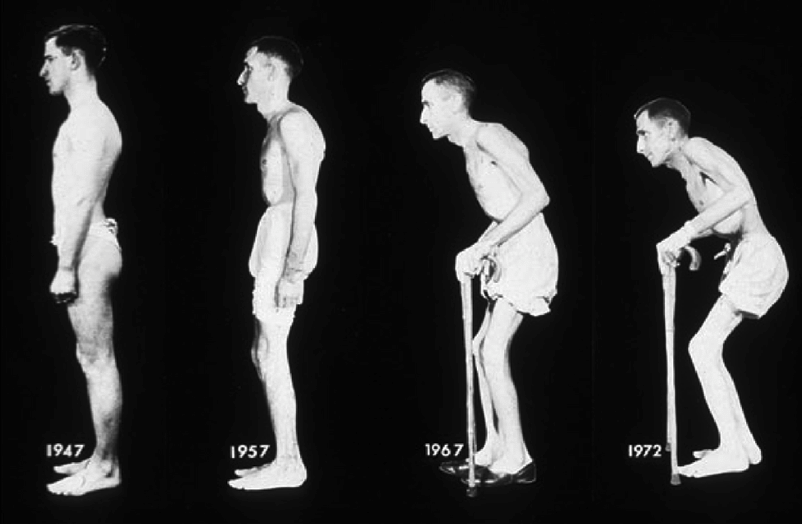
The help would take the form of Chiropractic adjustments and guidance, but the prognosis was not quite so simple. AS is a progressive disease but the rate and characteristics of that progress is variable. Most finish up with total fusion of the SIJs and spine, and many fold over into extreme kyphosis. (see below)
I started adjusting Leigh using SOT and AMCT which produced very good results with both a marked reduction in pain and increased ROM. He was largely stable for around 10 years but the stiffness began to gradually worsen. For the subsequent 10 years I had to add manual adjustments to the thoracic region because the Activator was no longer giving him relief. That worked well but with decreasing efficacy up until 2009 when I started using the Impulse iQ.
For those unfamiliar with the iQ, it’s a hand held electronic instrument that produces a measured thrust. Once the thrust has been produced the accelerometer inside the instrument measures the rebound, feeds that information back to the CPU, which then moderates the following thrust according to that measurement. This cycle is repeated until the target tissue or joint releases and resumes its normal motion at resonant frequency. Simply put, the instrument cycles though “test, treat, test, treat, test….” until normal joint or tissue mobility is restored. The beauty of this process is that the patient can see, feel and hear the changes as they happen. This factor alone makes an enormous positive difference to the patient experience and thereby increases patient confidence and compliance.
Using the iQ allowed me to continue adjusting Leigh well past the time when his spine had completely fused from the SIJs to the lower cervical region. You’re probably wondering how could I adjust his spine when the AS had fused it.
This is where we need to let go of our simplistic “bone-out-of-place” notion and understand that we’re not pushing bones from Point A to Point B. We are changing joint motion, resetting the baseline contraction rate of the intrinsic micro-muscles, enhancing circulation in and around the joint, altering lymphatic flow around the joint, breaking adhesions, resetting the proprioceptors and probably a lot of other things that we don’t yet fully understand.
The regulated cyclic pulsing of the iQ has made a phenomenal difference to Leigh. I still adjust him with it to this day and the results have been extraordinary. He gets instant relief from the pain and stiffness that lasts around 2 weeks. He’s able to crawl around under his car, ride his bike, wriggle into the hull of his fishing boat, walk long distances, sit for long periods of time and generally get on with his life.
It would be nice to think that the AS somehow “went away” but as you can see from the X-rays below, it has not. Nor did he escape the “fun park of misery” that accompanies many of the arthritides. In Leigh’s case he got the full enchilada; joint fusion, uveitis and urethritis. As bad as that is, and really is bad, Leigh’s life is infinitely better with Chiropractic than it would’ve been without it.
Had he gone down the strictly allopathic road he would be given the ascending regime:
Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) – Ibuprofen, Naproxen
Tumor Necrosis Factor (TNF) Inhibitors – Adalimumab, Infliximab
Interleukin-17 (IL-17) Inhibitors – Secukinumab, Ixekizumab
Janus Kinase (JAK) Inhibitors – Tofacitinib
Corticosteroids – Prednisone
This is Leigh today, 35 years after the initial diagnosis

These are Leigh’s most recent X-rays


So what was the point of this Case?
Well, it wasn’t to see if you could diagnose a case of Ankylosing Spondylitis – hopefully you can all do that in your sleep (except for the students).
The main point of it was to show you the power of what Chiropractic can do, and that we have the knowledge and tools to change patients’ lives for the better, forever.
It was also to remind you not to allow your diagnosis to get railroaded by a “Headline Ailment” like cancer, heart disease, or as in Leigh’s case, an apparently incurable arthritic disease.
Finally it was encourage you. If you feel like you’ve reached the end of your abilities, or the patient is not responding as well as you’d hoped, keep looking, keep researching, keep hunting down whatever tool or technique you think might help them.
That being said, one of the most noble things you can say to a patient when you get to the bottom of your toolbox is “I’m sorry, I’ve given it everything I’ve got but I think you need to see (fill in the space). Let’s find someone who can help you take the next step”
Above all…. maintain your Honesty, your Excellence, and your Kindness

